Osteoarthritis finding sheds light on HA injection controversy
By Syl Kacapyr
A discovery by Cornell bioengineers is shedding new light on the controversy surrounding a common treatment for osteoarthritis that has divided the medical community over its effectiveness.
Osteoarthritis occurs when the protective cartilage on the ends of bones wears down, allowing the bones to rub together and causing pain. Injections of hyaluronic acid (HA) are a common treatment of osteoarthritis of the knee – a condition that affects 27 million Americans, according to the Centers for Disease Control and Prevention. The injections replace the depleted HA that naturally would lubricate the joint.
There are eight different HA products sold in the U.S. with annual sales approaching $1 billion. While all of these products are approved by the Food and Drug Administration, studies have produced mixed results on their effectiveness, leading researchers and doctors to question how HA actually functions in the body.
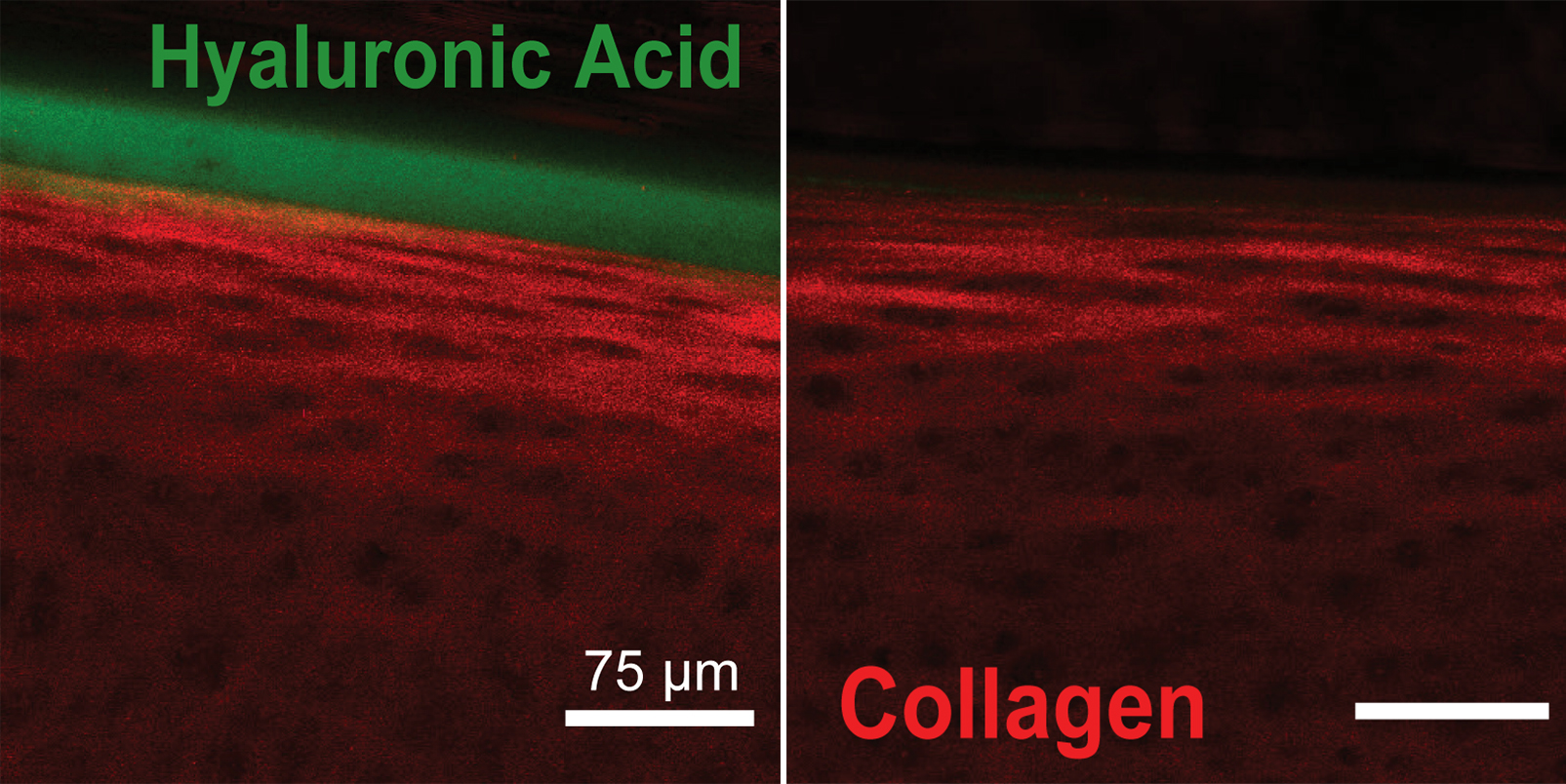
A research group led by Lawrence Bonassar, professor of biomedical engineering, and graduate student Edward Bonnevie has discovered that another molecule, lubricin, helps anchor HA at the tissue surface, which, in turn, helps to move cartilage into a low-friction regime.
“The implication of this finding is that the efficacy of HA treatment might depend on how much lubricin is in the joint at the time of injection, which could explain why clinical trials of HA have such variable outcomes and may also suggest new formulations of HA that might be even more effective in the clinic,” said Bonassar.
The study, published Nov. 24 in the journal PLOS ONE, examined how multiple formulations of HA lubricated cartilage and found that they all worked by a similar mechanism, “one that is very similar to how a car hydroplanes on a wet road,” said Bonassar. Essentially, the viscous HA solutions form pressurized films that lower the friction coefficient of cartilage, particularly at higher sliding speeds. “For many years, people doubted that this mechanism could happen in cartilage because the tissue is both flexible and porous. In this paper, we show definitively that cartilage can move to this low-friction domain in the presence of highly viscous HA solutions,” said Bonassar.
Scientists from Fidia Farmaceutici S.p.A. co-authored the study and used the results to bioengineer a new derivative of natural HA. This new HA derivative, known as HYADD4, has been approved by the FDA for clinical use in the U.S. and will be marketed under the name Hymovis starting in March.
“We are proud to have contributed to this important discovery. This research is a result of Fidia’s long-term focus and commitment to HA research and development. With Hymovis, we now have a new generation hyaluronic acid with increased elasticity, viscosity and residence time in the joint,” said Dr. Cynthia Secchieri, director of research and development at Fidia Farmaceutici S.p.A.
Syl Kacapyr is public relations and content manager for the College of Engineering.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe