Softening of tumor tissue could aid in cancer drug delivery
By Tom Fleischman
As a tumor grows, the environment surrounding the cancer stiffens, as does the tumor itself. And according to new Cornell research, there is another effect of that stiffening: damage to the blood vessels of the tumor.
In a study published Dec. 22 in the Proceedings of the National Academy of Sciences, a Cornell team found that the stiffening of the matrix surrounding a metastatic tumor plays a key role in the vascular makeup of the tumor. And it’s that unhealthy vascular makeup that promotes tumor growth and mobility by keeping drugs out.
The team – led by Cynthia Reinhart-King, former associate professor of biomedical engineering, lead author François Bordeleau, postdoctoral researcher in the Reinhart-King group, and their collaborators from five Cornell departments or schools, including Weill Cornell Medicine – propose a structural solution to seemingly a chemical problem. Their report is titled “Matrix Stiffening Promotes a Tumor Vasculature Phenotype.”
For years, Reinhart-King said, the idea was that starving tumors would kill off their blood vessels. While that works in some cases, in others it only serves to make the tumor more aggressive, she said.
“There are ways tumors can grow in the absence of those nutrients, and they get more aggressive,” she said. “They also stop responding to some chemotherapeutics and some radiation treatments.”
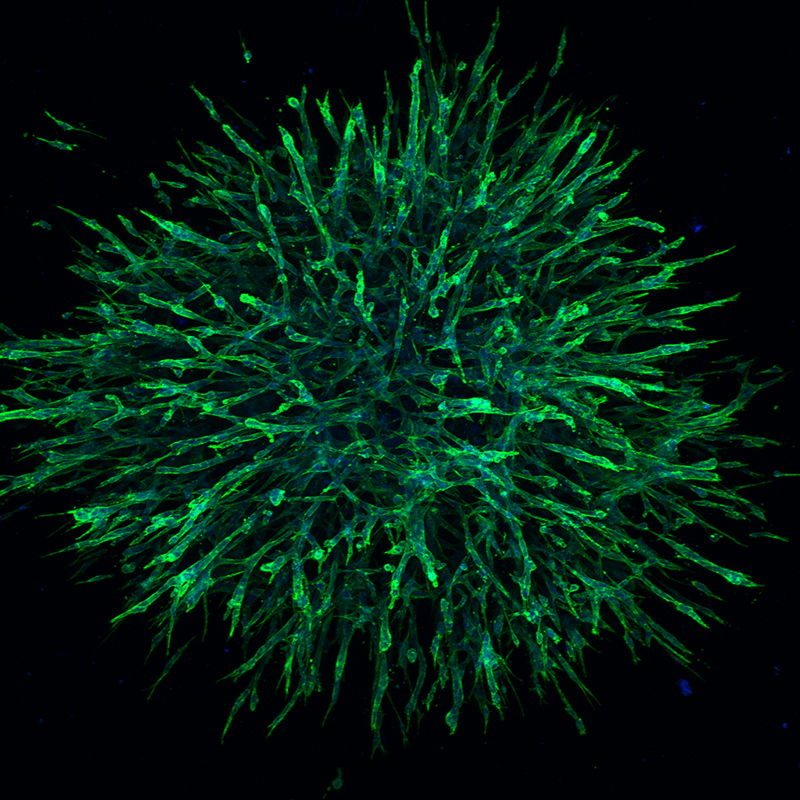
A metastatic tumor’s blood vessels tend to be malformed and more permeable than blood vessels in healthy tissue. For this reason, fluid tends to leak from the vessels, building up pressure inside the tumor that prevents drugs from getting to their target.
“Basically, as fluid leaks out of the blood vessels, it causes high pressures to build up in the tumor. These high pressures can cause blood flow to stall or even reverse and vessels to collapse,” Reinhart-King said. “So fluid, including the drugs, cannot reach the tumor tissue.
Dr. Duane Hassane, assistant professor of computational biomedicine in medicine at Weill Cornell Medicine, said that through genomic analyses, the group gained insight into how mechanical changes in the tumor impact vascular biology.
“Going forward,” Hassane said, “genomic information will enable us to optimize the administration of anti-cancer drugs in the context of tumor mechanics so as to maximize the impact of cancer therapies.”
Unlike in previous work in this area, Reinhart-King and Bordeleau see the vascular breakdown as a product of the stiffening of the tumor and its matrix, which triggers proteins in cells to alter vascular growth and integrity. Previous work has targeted chemical factors, in particular vascular endothelial growth factor.
“The idea that you would want to restore barrier integrity and help blood vessels is not a new one,” Reinhart-King said. “The idea that we discovered is that it’s controlled through matrix stiffness.”
But by promoting healthy vasculature through a softening of the extracellular matrix, she said you’re actually using the tumor itself as a conduit for delivering cancer-killing drugs.
“What we show,” Reinhart-King said, “is that we can drive a lot of the same behaviors that are typically thought to occur due to chemical changes, by changing the mechanical properties of the tumor.”
Reinhart-King and Bordeleau showed last year, also in PNAS, how the mechanical properties of the tumor influence how cells produce protein variants characteristic of the tumor vasculature. Together, these studies highlight how the mechanical properties of the tumor alter the cells within the tumor in several interconnected ways.
Other collaborators included Lawrence Bonassar, professor of biomedical engineering; Jonathan Butcher, associate professor and associate director of biomedical engineering; and Robert Weiss, professor of molecular genetics in the College of Veterinary Medicine.
Reinhart-King and Bordeleau are now at Vanderbilt University; all the work was conducted at Cornell, with sequencing studies done at Weill Cornell Medicine.
This work was supported by grants from the National Institutes of Health and the National Science Foundation, as well as the Scholarships for the Next Generation of Scientists program from the Cancer Research Society (Bordeleau). Imaging data was acquired at the Cornell Biotechnology Resource Center, which is a state-designated Center for Advanced Technology.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe