$2.5M grant funds research on tuberculosis treatment
By Krishna Ramanujan
Cornell researchers are investigating compounds they identified that offer hope for effective new drugs against tuberculosis.
“Tuberculosis now kills more people than HIV every year. It’s the leading infectious disease on the planet in terms of human death,” said Brian VanderVen, assistant professor of microbiology and immunology in the College of Veterinary Medicine, and principal investigator of a new five-year, $2.5 million National Institutes of Health grant to study new compounds that he and colleagues identified and described. “We need new anti-tuberculosis antibiotics that work better and faster.”
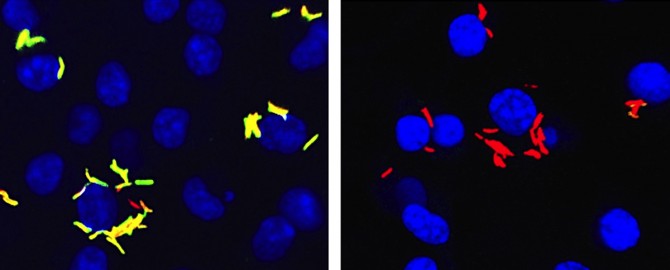
The bacterium, Mycobacterium tuberculosis can persist in humans for decades, hiding from the host’s immune system by living within cells called macrophages, a white blood cell type that normally rids our bodies from invading bacteria. The funds will support research to uncover the basic mechanisms of how these compounds work to suppress Mycobacterium tuberculosis inside macrophages.
“The real breakthrough with these compounds that we describe is that they specifically work against the bacteria when it’s living in a macrophage,” VanderVen said. “This is the first class of compounds of this type that shuts down Mycobacterium tuberculosis metabolism when the bacteria are growing in a macrophage.”
Inside macrophages the bacteria switch their metabolism to use cholesterol and fatty acids, and these new compounds inhibit the bacteria’s ability to use these lipids.
Over the span of the grant, VanderVen and collaborators, including Holger Sondermann, associate professor of biophysics in the College of Veterinary Medicine, hope to understand the precise mechanism of action of these compounds and evaluate the potential of these types of lipid inhibitors as therapies.
“TB treatment requires six to nine months of daily dosing,” VanderVen said. “We really want to shorten treatment, and including something like a compound that inhibits bacterial growth inside its host cell might make current treatments better.”
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe