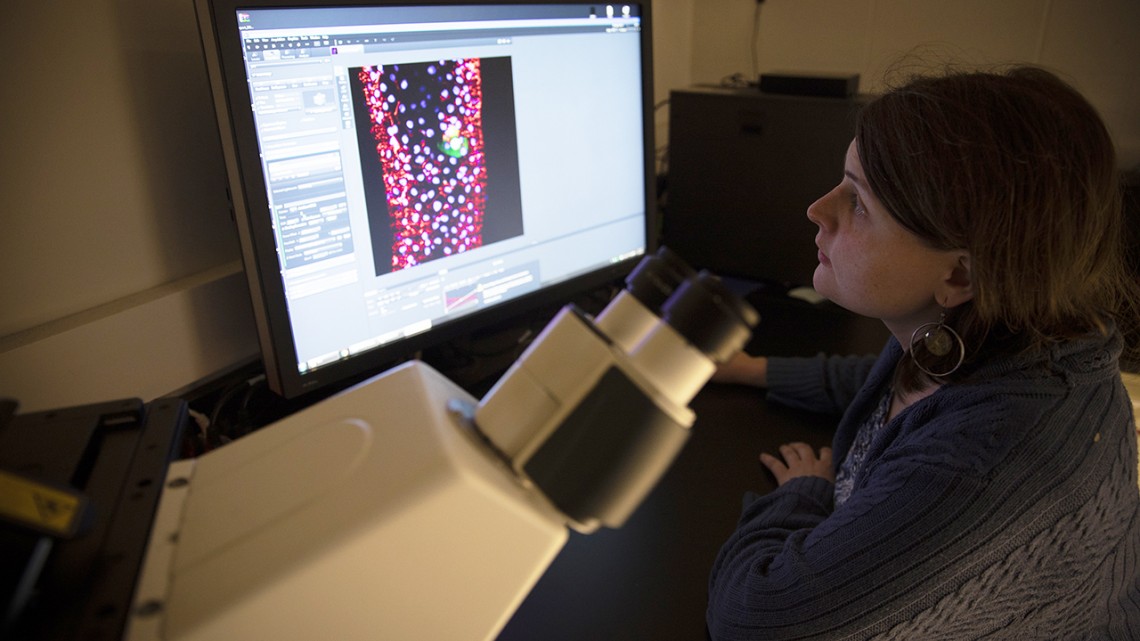
Bretta Hixson, a graduate student in the lab of Nicolas Buchon, examines the structure of a fruit fly midgut using confocal microscopy.
Researchers explore gut biology similarities across species and colleges
By Joe Wilensky
Praveen Sethupathy ’03, associate professor of biomedical sciences in the College of Veterinary Medicine, and Nicolas Buchon, assistant professor of entomology in the College of Agriculture and Life Sciences, collaborate in the study of gut biology, gut microbes, and intestinal stem cells and their function and response to environment, diet and disease. Sethupathy studies microRNAs and the gut in mouse models and human organoids and Buchon studies host-microbe interactions and stem cell biology in the five-millimeter-long GI tract of the fruit fly (drosophila) or in disease vector mosquitoes.
Sethupathy also is a member of the provost’s Genome Biology Task Force.
How does your collaboration work, and how did it develop?
Sethupathy: I was recruited to Cornell from the University of North Carolina, Chapel Hill. Because our lab mostly uses the mouse as a model system, I was looking for researchers on campus with complementary expertise in other species, whether it be canine, zebrafish or fruit fly. And that’s when I came across some of Nicolas’ research. I started reading up on some of his work, and then connected with him to see if there might be some unique opportunities to integrate his fruit fly research with our ongoing mouse- and human-oriented studies.
There are 530 or so million years, evolutionarily speaking, separating fruit flies and humans – and that’s the thing I find the most fascinating about the collaboration. Because, despite that amount of time, we find some mechanisms at the molecular level that are very strongly conserved … and appear to be critical for controlling biological processes in the gut that are fundamental to health and disease.
Buchon: We were already in contact through a common collaborator (John Rawls at Duke University, who studies gut biology in zebrafish), and we didn’t even know it. When it was announced that Praveen would be hired, it was a great opportunity because our teams are really, really connected and our work easy to combine. We each have our own desire to look at gut function and our collaboration allows an evolutionary perspective coming from different organisms.
Sethupathy: The collaboration really did start with a shared interest to see what kinds of commonalities, and differences, there were across these three species in terms of how the gut functions and responds to stress.
What does so much commonality in the gut biology among these species mean?
Buchon: It means that the gut is one of the most ancestral organs, and as a consequence most organisms inherited its ancient function. When you start to develop a complex organism, you start with the digestive system, and all digestive tracts face similar challenges: acquiring nutrients, hosting microbes, et cetera.
Sethupathy: What we’re identifying are specific molecules that have retained the same functionalities over hundreds of millions of years of evolution. It really speaks to something fundamental about the activities of these molecules within the cells of the gut.
Buchon: There is now a renewal of interest in the gut as an organ, beyond just digestive physiology, because of the microbiome revolution. Hosting gut microbes is a crucial, and conserved, function of the digestive system.
Our labs are both interested in understanding how stem cells build that organ (intestinal stem cells rebuild the entire inner lining of the gut every 3-5 days or so in humans) and respond to cues from the environment, such as nutrition or microbes. This means that depending on what you eat and the microbes you host, you won’t build the same organ! How these stem cells behave is important for understanding diseases like cancer, inflammatory bowel disease and diabetes … It’s also deeply evolutionarily rooted.
Sethupathy: That brings us to the other part of my lab, in which we focus a lot on these little “critters” called microRNAs. As the name suggests, they are very small molecules that function as RNAs instead of becoming proteins. And over the last decade and a half, the RNA field has championed this idea that microRNAs are very important in responding to environmental stressors, bringing the system back to some kind of equilibrium or homeostasis.
And that’s actually why we got interested in the gut … [it’s] such a dynamic environment, constantly changing. And, what's more, the cells of the inner lining of your gut are completely new each week. These cells have to digest food, take in nutrients, keep out pathogens, communicate with other organs, and respond swiftly to all sorts of stressors – all of these activities are shared between mouse, human and fruit fly.
What about stem cells holds the promise of what you may discover?
Sethupathy: This is one of the most exciting areas of research in gut biology. Crudely speaking, we can think about stem cells as two types: embryonic stem cells and adult stem cells. The latter are cells that can become multiple different types of cells, but generally only those within the organ in which they’re embedded. So an adult intestinal stem cell can become many other kinds of specialized cells, but all of them remain in the gut and work together. When we talk about the lining of the gut getting renewed on a weekly basis, that’s driven by a population of highly proliferative adult intestinal stem cells.
How those cells respond to different kinds of environmental cues, how vulnerable they are to certain kinds of stressors, and how other nearby specialized cells can compensate for that vulnerability, are all questions of significant interest to us because they are critical for understanding diseases like diabetes, inflammatory bowel disease, and cancer.
The fruit fly, Drosophila, presents an advantage for testing hypotheses in part because of the much more rapid life cycle.
Buchon: Drosophila is like a Swiss Army knife of genetics. It reflects a hundred years of accumulation of tools to manipulate genes at will. And very importantly, it allows to look at gene function in vivo, inside a living organism.
Stem cells are important in multiple ways. They’re important for tissue repair and re-growing an organ that faced some damage, but you can consider the reverse: If they start to divide too much, you’ll have tumors; or even initiate a cancer. With that in mind, understanding how physiology alters normal stem cells’ behavior will probably lead to understanding how, these environmental parameters, nutrition and your gut microbes can influence health and disease.
Your gut is also one of the organs that produces the most hormones in your body – it’s actually a major orchestrator of the body’s endocrine system. So as all those environmental factors change the actual organ you build, they will also have repercussions on physiology way beyond the gut itself.
What have you each learned from the other?
Sethupathy: I’ve learned most about actual species-specific differences. I bring to the table certain assumptions about the way things work, because I’m embedded in a community of people who are focused on mouse and human biology. But when I talk with Nicolas I realize that’s not necessarily the way that the Drosophila field looks at things. And that widens my horizons and makes me a better scientist.
This expansion of the mind leads not only to better science but also challenges us to be better communicators. Because of Nicolas I might be more cognizant of some of the differences in assumptions and jargon between Drosophila and mammalian gut biologists.
Buchon: The same is true for me – our collaboration has really expanded my horizons. I think we learn both from the similarities and from the differences of our systems. Both make us understand what’s core to gut physiology and what’s more specific to one organism. It really helps approach our questions with a fresh eye.
Are you near a watershed moment, a new level of understanding in your fields?
Sethupathy: One emerging and important concept right now in gut biology is this notion of plasticity. We like to discretize, we like to say, “This cell does this thing.” “This cell does this other thing.” But what we’re finding is that it’s highly context-specific. So, depending on the environmental condition, cells can change their behaviors – sometimes even revert into other cells.
It has been shown recently that several different specialized cell types of the gut possess the underlying capacity to revert back into a stem cell if needed.
Which cells really are able to do this best, and why? How are they able to do this, and what kinds of triggers activate them? Some of these triggers we already know about, like radiation therapy and chemotherapy, which are of course of tremendous biomedical significance.
Buchon: The gut is a center for decision making – it makes decisions based on the environment. And that affects your whole physiology. Currently, we don’t know how those decisions are made. Through genetics and cell biology, we try to understand, how does the gut “think?” How does it make its decisions to adjust your physiology? You can see how that can be crucial for health and disease, because if we don’t know how the organ makes its decision, we can’t influence these decisions. So that’s one of the exciting promises there.
Praveen, as a member of Provost Michael Kotlikoff’s Genome Biology Task Force, what is your perspective on Cornell’s collaboration efforts?
Sethupathy: I think our collaboration is exactly the kind of thing that the provost is thinking about. When he says “radical collaboration,” one of the major things he has in his mind is how can we reduce the administrative, bureaucratic and other kinds of barriers to allow people – cross-school, cross-department, cross-institution, cross-campus – to work together effectively and feel like they’re being supported by not only their home departments, but the institution as a whole? Lower the energy needed to climb over those walls and get work done together.
I think genome biology is particularly conducive to this kind of radical collaboration initiative because its home isn’t in any one department. Anybody can do genome biology if they’re in the life sciences. Even people in chemistry who are outside of life sciences have an investment in genome biology.
And so it’s really neat – you’ve got faculty members from engineering, chemistry, nutrition, genetics, molecular medicine, evolutionary biology, plant sciences, computational biology, et cetera, all serving together on this committee to cement Cornell’s leadership position in genomics.
That was one of the things that sold me on getting recruited here – the opportunity to participate on this task force and help shape genome biology research on campus and beyond.
Nicolas, what have your Cornell collaborations been like?
Buchon: I was unaware of these task forces before I came to Cornell, but it was already striking to me that Cornell is probably the most collaborative environment I’ve encountered. I do collaborate with people in every one of those biology departments. And that’s mostly a question of local culture. However, this culture of collaboration needs nurturing, and I think these initiatives really help maintain this dynamic. I believe it is one of the strengths of Cornell.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe