Cornell's Torres helps monitor path of avian flu virus as threat to human population grows
By Krishna Ramanujan

If a virulent strain of avian influenza ever struck the U.S. poultry industry, this country probably would fare better than many other nations due to careful biosecurity procedures in force.
But if the virus develops an ability to pass from one human to another, the United States would have far less protection as the world possibly faces one of the worst flu pandemics in history.
Among the U.S. health officials watching the progress of this extraordinarily active virus (known as H5N1) as it infects chickens in Asia and waterfowl in Russia, is Alfonso Torres, director of the Animal Health Diagnostic Center and associate dean for veterinary public policy at Cornell University's College of Veterinary Medicine.
"The fear is that if the virus changes or recombines with a regular human flu, the virus may acquire the ability to be effectively transmitted from human to human, then it could become the big pandemic that everyone is very concerned about," he says. As a consultant, Torres has held high-level policy discussions on avian flu with the U.S. Department of Agriculture (USDA) and NATO, among others.
For now, the United States, like the rest of the Western world, can only watch and prepare. Since January 2004, the known human cases of avian flu have all struck in Southeast Asia -- out of 120 patients requiring treatment, about half have died. All of these infections were contracted from chickens, with the exception of a case in Thailand where the source is unclear.
A natural reservoir for the avian flu virus is migratory waterfowl, and infected birds have been found in Mongolia, Kazakhstan and Russia, raising concern in the U.S. as the disease moves west. Although waterfowl do not appear to be playing a big role in poultry and human transmissions right now, they are being closely monitored.
"When experts look at the maps of the areas affected by avian influenza in Asia and they look at the flying pathways of migratory waterfowl, there is not an overlap," Torres observes. Although waterfowl are the natural reservoir for all types of avian flu -- meaning they are long-term hosts of these viruses and pass them among each other, but often may not get sick or they develop mild infections -- Torres says, "Waterfowl, at this point in time, are not the culprit for what is happening in Asia."
Rather, the disease has spread in Asia in backyard and low-tech poultry and duck production areas where people transport infected chickens atop cars or on motorbikes to markets. There, sick birds can infect other birds that then return home unsold. Also, people who handle uncooked meat and infected birds can spread the flu virus from bird to bird.
But in Asian poultry farms that use modern biosecurity practices, like those in the United States that prevent infectious diseases from spreading through flocks, the disease has not spread. U.S. biosecurity regulations serve to minimize contact between poultry and outside materials that could bring disease. For example, measures can require poultry farm workers to take showers upon entering a production facility and when they move between birdhouses on the farm, and restricts them from owning pet birds at home and from hunting ducks and other waterfowl.
As long as the disease stays primarily a bird flu, officials have some control, says Torres, a former U.S. chief veterinary officer and director of the Plum Island Animal Disease Center, a high-security animal laboratory previously operated by the USDA but now part of the Department of Homeland Security.

While H5N1 strain most concerns researchers because of its virulence and ability to be transferred from birds to people, all strains that include the H5 and H7 proteins are now monitored because they are most commonly affect poultry and they could potentially mutate into more virulent, contagious forms.
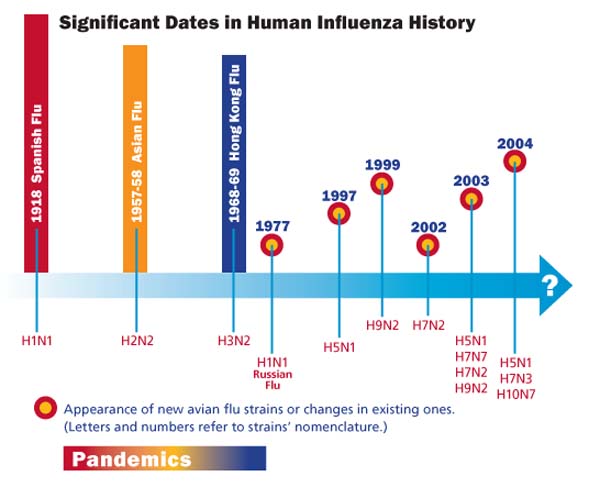
International policy-makers are debating whether to routinely vaccinate poultry with H5 or H7 avian flu viruses. They are also deciding whether to include H5N1 in regular human flu vaccines, which the U.S. government might also stockpile. Without advanced stockpiling, vaccine production takes many months to ramp up. But creating an effective vaccine in advance of a flu season is a little like hitting a moving target, as flu viruses notoriously change, either by slow genetic drifting through small mutations that add up over time or by sudden shifts where two virus strains, for example avian and human flu, swap genetic material in a commonly infected host cell. Torres believes that a slow drift likely led to the first human case of avian flu in 1997. Either way, flu vaccines are never sure-fire.
Pharmaceutical antiviral medications, like oseltamivir (Tamiflu), can also control the disease in humans by affecting the flu virus' ability to multiply in the patient, minimizing its effects and allowing the body's natural defenses to get rid of the infection. Government policy leaders are considering contracting with drug companies to make millions of doses of such antivirals.
However, there is concern that indiscriminate use of the drug would allow the H5N1 virus to develop resistance to the medication, Torres says. One strategy could be to target only certain populations, such as healthcare workers and first responders including ambulance drivers, firefighters and police officers.
However, says Torres, the world still has much to learn from the 1918 flu pandemic that killed more than 20 million people. "One thing that happened in the so-called Spanish flu was a high mortality rate among the healthiest individuals," he says. "The healthier they were, the more susceptible they were."
That's because the Spanish flu virus caused an exaggerated immune-inflammatory response in which cells release chemicals that affect the permeability of blood vessels and cause fluids to flood the lungs, leading to suffocation within hours.
Torres is currently working with an independent policy and research think-tank in Washington, D.C., to organize a conference early this winter to bring together experts from public health, animal health, wildlife management and the poultry industry for a larger discussion on avian flu.
"We need to have that four-way conversation," he says. "We cannot do this in a vacuum."
Experiences with the West Nile virus, SARS and monkey pox have taught health officials that in order to battle epidemics, there must be coordination and dialogue among experts in a variety of medical disciplines in conjunction with industry and the private sector, Torres says.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe