Improving care of hospitalized patients with HIV in Tanzania
By Karen Hopkin
Researchers at Weill Cornell Medicine have shown that three months of social worker follow-up support to people hospitalized with HIV in Tanzania had health benefits at low cost. The protocol shortened the time it took participants to attend an HIV clinic and to start on antiretroviral therapy after discharge.
However, the study published in JAMA on March 6 found that the care benefits didn’t translate to a decrease in mortality after one year. They compared a group that received extended case management intervention with a control group receiving standard care and determined both had the same mortality rate – in each group, 17% of participants died.
“The findings show that it’s not enough to get people into the clinic and started on antiretroviral therapy because our intervention was highly effective at doing that,” said lead author Robert N. Peck, associate professor of medicine and pediatrics at Weill Cornell Medicine. “Unfortunately, the intervention did not have an impact on mortality. So, if we want to improve survival and reduce these AIDS-related deaths, we’re really going to need to do more.”
An accompanying editorial in JAMA noted that the study is among the first clinical trials focused on hospitalized people with HIV to demonstrate several potential, clinically meaningful benefits. “The Daraja intervention makes a valuable addition to the compendium of options that can sustainably and equitably meet people ‘where they are at’ at a time when they may be in greatest need,” the editorial stated.
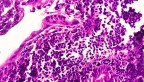
Approximately 630,000 people still die of AIDS-related causes each year, with two-thirds of these deaths occurring in sub-Saharan Africa, according to UNAIDS. Individuals who are hospitalized with HIV are particularly at risk because they often arrive with severe immunosuppression and advanced opportunistic infections, including tuberculosis and cryptococcal meningitis, a fungal infection that often spreads to the brain.
To improve treatment outcomes, Peck worked with colleagues at the Weill Bugando School of Medicine, the Mwanza Interventions Trial Unit in Tanzania and Lisa Rosen-Metsch at Columbia University, designing a protocol that addresses the barriers to care typically encountered in Tanzania, including stigma, lack of social support and reliance on traditional medicines. The senior author on the paper was Saidi Kapiga, scientific director of the Mwanza Intervention Trials Unit.
They dubbed the intervention Daraja, from the Kiswahili term for bridge, “because we saw the intervention as bridging the gap between the hospital, the HIV clinic and better health for our patients,” he said.
Peck and his team enrolled 500 hospitalized people with HIV across 20 sites, half of which were randomized to receive five sessions with a social worker. These interactions, completed within three months of discharge from the hospital, included a home visit to assess participants’ resources, as well as meetings at the HIV clinic to help them navigate the HIV care system and facilitate making antiretroviral therapy part of their daily lives.
The early results were encouraging. By the end of the first month, 92% of people in the intervention arm had attended the HIV clinic versus 75% of those in the control arm. The outcomes also appeared to be long-lasting. At the end of one year – nine months after the intervention had ended – 87% percent of those who received Daraja were still visiting the clinic versus 76% of those who did not. And more of the Daraja recipients saw a suppression of their viral load.
The program was also highly cost effective. Sean Murphy, professor of public health sciences at Weill Cornell Medicine, crunched the numbers and found that Daraja’s price tag totaled about $22 per person.
Despite the benefits of the program, the researchers noted that some participants were already at advanced stages of HIV which made increasing survival rates difficult to achieve. “For that subset of participants, I think the answer is better prevention, as well as earlier diagnosis and treatment,” said Peck, who is also a member of the Center for Global Health at Weill Cornell Medicine.
Others are not successfully treated for their opportunistic infections during their hospital stays. “If we really want to reduce mortality, we also need to improve the clinical care in the hospital,” said Peck, who would like to see a clinical trial that combines enhanced clinical care with a case management intervention like Daraja.
In the meantime, Peck is continuing to follow the study’s current cohort for an additional year. “We already know that more of those in the intervention group were attending clinic, taking antiretroviral therapy, and virally suppressed,” he said. “So, although Daraja did not reduce mortality in the first 12 months, I think it might improve health in the longer term.”
This study was supported by the National Institute of Mental Health of the National Institutes of Health (NIH); the National Heart, Lung, and Blood Institute; and the NIH Fogarty International Center.
Karen Hopkin is a freelance writer for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe