Bacteria links Crohn's disease, arthritis, researchers find
By Jen Singer
Patients with Crohn’s disease, a type of inflammatory bowel disease (IBD) that causes abdominal pain and diarrhea, can also experience joint pain. In Crohn’s disease, which affects about 800,000 Americans, the immune system can attack not only the bowels, but the musculoskeletal system as well, leading to spondyloarthritis, a painful condition that affects the spine and joints.
Research published Feb. 8 in Science Translational Medicine helps explain the connection between these seemingly unrelated symptoms, and could help physicians identify Crohn’s disease patients who are more likely to develop spondyloarthritis, enabling them to prescribe more effective therapies for both conditions.
New technology helped the researchers identify a type of E. coli bacteria found in people with Crohn’s disease that can trigger inflammation associated with spondyloarthritis, according to the study led by principal investigator Dr. Randy Longman and scientists from the Jill Roberts Center for Inflammatory Bowel Disease at NewYork-Presbyterian and Weill Cornell Medicine and the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine, microbiologists at Cornell’s College of Veterinary Medicine, and rheumatologists at the Hospital for Special Surgery (HSS).
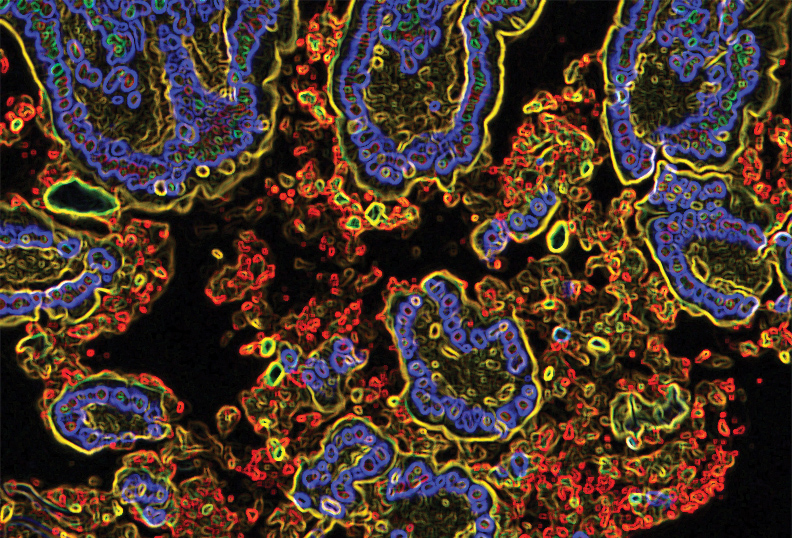
The researchers used fecal samples from patients with IBD to identify bacteria in the gut that were coated with antibodies called immunoglobulin-A (IgA) that fight infection. Using flow cytometry, in which fluorescent probes are used to detect IgA-coated bacterial species, the researchers discovered that IgA-coated E. coli were abundant in fecal samples from patients with both Crohn’s disease and spondyloarthritis. Using patient samples and mouse models, they then linked these bacteria to cells that help regulate inflammation, known as Th17 cells, in people with autoimmune disorders.
“Our findings may allow us to develop diagnostic tools to stratify Crohn’s patients with spondyloarthritis symptoms as well as patients at risk,” said senior author Longman, assistant professor of medicine and director of the Jill Roberts Institute Longman Lab at Weill Cornell Medicine.
The investigators found that patients with Crohn’s disease and spondyloarthritis had higher levels of Th17 cells and that a protein called IL-23 triggers their activity. With the recent FDA approval of an anti-IL-23 medication for Crohn’s disease called ustekinumab, the findings may help physicians select therapies that target symptoms of both the bowels and the joints in these patients, Longman said.
“Just sequencing the gut flora gives you an inventory of the bacteria, but does not tell you how they are perceived by the host immune system,” said co-author Dr. Kenneth Simpson, professor of small animal medicine at the College of Veterinary Medicine, whose laboratory characterized theE. coli identified in the study. “This approach is giving you a functional readout versus just an inventory.”
Longman led the translational study along with co-author Dr. Ellen Scherl, director of the Roberts Center at NewYork-Presbyterian and Weill Cornell Medicine and the Jill Roberts Professor of Medicine at Weill Cornell Medicine, in collaboration with HSS rheumatologists and co-authors Dr. Lisa Mandl and Dr. Sergio Schwartzman. Initial funding for the work was provided by a pilot seed grant to foster collaborations between researchers in Ithaca and New York City, and has since been funded by the New York Crohn’s Foundation, the Charina Endowment Fund, the Center for Advanced Digestive Care, the Jill Roberts Institute for Research in IBD and the National Institutes of Health.
“We knew there was smoke, but we didn't know where the fire was,” said Simpson, who added that each collaborator provided unique expertise to uncover the findings. “If we can block the ability of bacteria to induce inflammation, we may be able to kick Crohn’s disease and spondyloarthritis into remission.”
Longman added: “In IBD therapy, this is a step toward precision medicine – to be able to clinically and biologically characterize a subtype of disease and then select the medicine that would best fit the patient with this type of inflammation. The results of this innovative study will start to inform our decision of which of our available medications will give the best chance of helping the individual patient.”
Jen Singer is an editorial consultant for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe