Precision medicine, immunotherapy discussed at Weill Cornell Medicine
By Jamie Kass
Within the vast portfolio of research at the National Cancer Institute (NCI), its new director is paying close attention to advances in precision medicine and immunotherapy – two approaches that have the potential to reshape the way physicians treat cancer.
“Precision medicine is really going to change how we do oncology,” said Dr. Norman Sharpless during a talk at Weill Cornell Medicine March 15. “It’s going to force us to face the fact that cancer is not one disease but thousands of diseases.”
Speaking to faculty, staff and students at a packed Uris Auditorium, Sharpless shared his impressions as a new NCI director – he began his tenure in October 2017 – and highlighted work the institute is spearheading to drive new discoveries in cancer care.
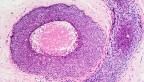
That includes the NCI-MATCH Trial, a precision medicine cancer treatment clinical trial that accrued patients at nearly 1,100 sites nationwide, including Weill Cornell Medicine. Patients have their tumors genetically sequenced and are assigned a therapy specifically targeted to their genetic lesion, if such a therapy is available. Preliminary results of the more than 30 different treatment arms, or groups of people receiving a particular treatment, suggest a greater role for genomic sequencing in determining therapeutic approaches.
“Even for cancers like breast cancer and gallbladder cancer, where you might not recommend next-generation sequencing, you can discover lesions that can drive one to a new therapy,” Sharpless said. The NCI-COG Pediatric MATCH trial adds genetic testing that can reveal inherited cancer predispositions, which can help physicians advise about the possible need to test other family members.
Genomic sequencing may also help identify patients who are good candidates for immunotherapy, a new therapy that uses immune cells to fight cancer. While immunotherapy has joined surgery, radiation and chemotherapy as vital cancer treatments, the technique is not without its challenges.
“It really is new, exciting and hot,” Sharpless said, “but most patients are still not benefitting from immunotherapy, either because their tumors cannot be made to respond to their immune systems, or because we don’t know how to do it yet. In some patients, these therapies have been literally lifesaving, but there are still far too many patients who are not responding. The therapy still needs a lot of work.”
Sharpless described research led by Dr. Stephen Chanock, director of the Division of Cancer Epidemiology and Genetics at NCI, that analyzed vast amounts of data from The Cancer Genome Atlas, a catalog of mutations from thousands of patients. Chanock’s team found that tumor cells in many types of cancers have a large number of mutations in their DNA, rather than just one or two.
Previous investigations in melanoma and lung cancer patients have shown that numerous mutations predicted a good response to a type of immunotherapy drug called a checkpoint inhibitor. These results suggest we ought to be sequencing a lot more patients than we’re sequencing today, said Sharpless.
Basic research is key to making immunotherapy more effective. “This is why basic science is still really important to fund,” Sharpless said.
While funding has been robust over the past two years and Sharpless is optimistic about the future, he acknowledged that there are always more good ideas than funds to support them. “I asked my division heads what they would do in the next one, two or five years of their programs if they had the funding, and I got $300 million worth of great ideas,” Sharpless said.
Regardless of funding pressures, the National Institutes of Health has a mandate from Congress to do a better job of training early-stage investigators. At the NCI, that mandate has translated into an effort to ease the burden on young investigators seeking research funding. The Method to Extend Research in Time (MERIT) award provides two extra years of funding to first-time applicants when their research is deemed worthy of funding through an R01 grant, the traditional five-year grant awarded for investigator-initiated research.
“We’ve been told that getting your first R01 renewed is a key step to becoming tenured. And the people who had trouble with that, some of them have trouble because of life changes like motherhood,” Sharpless said. “People have told us that if they just had a little more time before they had to renew, that would be helpful. This was something we could do to support young women in their faculty development.”
For other cancer researchers looking for funding, the Cancer Moonshot may be the place to apply. This set of funds, appropriated to the NCI by Congress, includes $1.8 billion in funding over seven years.
“It is hard to find anybody in cancer research who doesn’t have an interest that’s matched by some of the Moonshot funding,” Sharpless said.
Jamie Kass is a science writer for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe