Potential therapy for aggressive type of colon cancer shows promise
By Bridget Kuehn
An experimental therapy showed promise as treatment for an aggressively spreading type of colorectal cancer in preclinical models, according to a new study by Weill Cornell Medicine investigators.
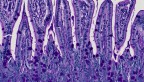
Mesenchymal colorectal cancer (mCRC) accounts for about one-third of all colorectal cancers. Targeted immune therapies aren’t effective against this form of cancer because the environment inside the tumor keeps immune cells that would kill the tumor cells at bay. But a team led by Maria Diaz-Meco and Jorge Moscat, who are both Homer T. Hirst III Professors of Oncology in Pathology at Weill Cornell Medicine, showed in a study published Dec. 15 in Cancer Cell that the accumulation of a molecule called hyaluronan is a critical step in forming mCRC tumors.
They also demonstrated that an experimental therapy targeting hyaluronan shrinks mCRC-like tumors in mice.
“We have unraveled one of the critical mechanisms driving this aggressive type of colorectal cancer, and we are proposing a potential therapy for patients who currently have few options,” said Moscat, vice-chair for cell and cancer pathobiology in the Department of Pathology and Laboratory Medicine and a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine.
“Our discovery also has important implications for preventing this type of colorectal cancer,” said Diaz-Meco, who is also a member of the Meyer Cancer Center.
A previous study by the team showed that patients with reduced levels of two enzymes called PKCz and PKCi are more likely to develop mCRC tumors and have worse prognoses. When the genes encoding these enzymes are shut off in mice, the animals develop mCRC-like tumors.
“Those two enzymes are the gatekeepers,” Moscat said. “When they are lost, it sets tumor formation in motion immediately.”
Using the animal model and single-cell analysis of their tumors, the team, including co-first authors Anxo Martinez-Ordoñez, a postdoctoral associate in pathology and laboratory medicine and Angeles Duran, an assistant professor of research in pathology and laboratory medicine, showed that one of the first steps in the process is the accumulation of hyaluronan, which begins before the tumors form. The hyaluronan attracts connective tissue cells called fibroblasts. These cells encourage the development of the most aggressive type of tumor cells and shut down the immune system's ability to kill the tumor cells, Moscat said.
But treating mice with mCRC-like tumors with an experimental therapy called hyaluronidase, which breaks down hyaluronan, shrank the tumors and allowed the immune cells to attack the tumor cells. Combining the targeted immunotherapies anti-PD-L1 and anti-CTLA-4 antibodies with hyaluronidase virtually eradicated mCRC tumors that had spread to the liver in the animals. Diaz-Meco explained that this is particularly exciting because liver metastases are common in patients with mCRC and are challenging to treat.
“Hyaluronidase makes the tumors susceptible to immunotherapy,” Diaz-Meco said.
The team also identified biomarkers that might help identify which patients with mCRC would benefit from hyaluronidase therapy. They are currently working with clinical partners to launch a clinical trial.
A clinical trial of hyaluronidase as a treatment for pancreatic cancer demonstrated that the drug is safe and has manageable side effects. But the therapy wasn't effective against pancreatic cancer. Diaz-Meco said they anticipate a better response in patients with mCRC because, unlike pancreatic cancer, these tumors have immune cells that although excluded from the core of the tumor, are present in its periphery and ready to be activated. Additionally, the dose they plan to test in patients with mCRC is equivalent to the amount used in the preclinical studies. Moscat explained that the preclinical studies on pancreatic cancer used much higher doses of the drug, which weren’t feasible for the human trial.
The team is also looking for ways to prevent mCRC from occurring or spreading. They hope to learn how the guardian enzymes are lost prior to the onset of cancer and if they can find treatments that block the production of hyaluronan to prevent cancer or its spread. Such treatments may be particularly beneficial for patients at high risk of colorectal cancer, such as those with ulcerative colitis or inflammatory bowel disease.
“If you can block the process by removing hyaluronan, you can prevent tumor formation or its spread to the liver, making it easier to treat,” Moscat said.
Dr. Maria Diaz-Meco and Dr. Jorge Moscat are co-founders, serve on the Board of Directors and hold equity in ZelamBio, Inc.
Bridget Kuehn is a freelance writer for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe