Technique shows how abnormal RNA splicing leads to disease
By Jim Schnabel
A technique that enables scientists to record gene mutations and patterns of gene activity in individual cells has been extended to cover RNA splicing as well, in a study led by researchers at Weill Cornell Medicine, the New York Genome Center and the Princess Margaret Cancer Centre in Toronto.
A better understanding of how aberrations in this process affect the development and behavior of cells is critical to understanding cancer and other diseases.
RNA splicing refers to the slicing up and reassembling of the RNA transcripts of active genes. An essential process in cells, RNA splicing is done on the transcripts of most genes, and for any given gene can yield up to several distinct proteins with at least subtly different functions. In the study, published Aug. 14 in Cell Stem Cell, the researchers modified one of their own cell-analysis methods so that it also yields information on RNA splicing – in a manner that makes it practical for the detailed analysis of tissue samples.
The team used the new method to reveal how mutations in genes that control RNA splicing lead to a type of blood cancer called myelodysplastic syndrome (MDS).
“Mutations that alter the RNA-splicing process underlie many cancers and other disorders,” said study co-senior author Dr. Dan Landau, associate professor of medicine in the Division of Hematology and Medical Oncology at Weill Cornell Medicine, a core faculty member of the New York Genome Center and an oncologist at NewYork-Presbyterian/Weill Cornell Medical Center. “This work allows us to track the impacts of those changes at an unprecedented level of detail.”
The co-first authors of the study were postdoctoral researcher Mariela Cortés-López, bioinformatics specialist Paulina Chamely, and postdoctoral researcher Allegra Hawkins, all of the Landau laboratory during the study; and Robert Stanley, a postdoctoral fellow at Memorial Sloan Kettering Cancer Center.
Landau and his laboratory study the origins and evolution of cancers as well as pre-malignant states that can lead to cancer. To facilitate their research, they have been developing new “single-cell multi-omics” techniques, which enable the profiling of multiple layers of information in individual cells. Single-cell techniques avoid the limitations of traditional methods that analyze bulk mixtures of cells.
In 2019, Landau and colleagues developed a technique called genotyping of transcriptomes (GoT), which, for the first time, enabled the high-throughput profiling of gene mutations and gene expression patterns in individual cells. In the new study, the team modified the RNA-sequencing method used for GoT so that RNA splicing information could be derived from it as well. The researchers also integrated what had been a separate method for detecting protein surface markers on single cells. The resulting “GoT-Splice” technique can thus record four distinct layers of information from individual cells.
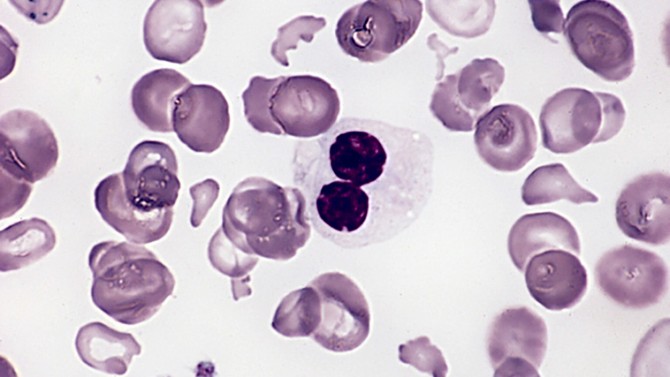
The researchers demonstrated the potential of GoT-Splice by using it to study a form of MDS in which patients’ bone marrow cells often contain mutations in SF3B1, a gene with a central role in the RNA splicing process. Patients with this MDS type have low levels of functional red blood cells, and their bone marrow shows a significant presence of immature red blood cells with characteristic abnormalities.
With GoT-Splice, the team analyzed tens of thousands of patient cells, detailing abnormal RNA splicing events in genes involved in cell survival, cell maturation and other key processes – and showing how these impacts varied across different subtypes of immature blood cell. The findings illuminated how the SF3B1 mutation, which arises in stem-like marrow cells, tilts the scales of the maturation process toward red rather than white blood cells, causes the characteristic abnormalities seen in immature red blood cells in MDS, and allows mutation-containing cells to proliferate and survive longer than they would otherwise.
“GoT-Splice has enabled us for the first time to link directly this SF3B1 mutation to the specific changes that are observed in these immature red blood cells in MDS,” said co-senior author Federico Gaiti, a postdoctoral researcher in the Landau laboratory during the study, now an assistant professor at the Princess Margaret Cancer Centre in Toronto.
Underscoring the clinical relevance of the findings, the researchers discovered that one of the genes whose normal RNA-splicing is disrupted by the SF3B1 mutation is BAX, a mediator of a key anticancer mechanism called apoptosis. BAX mutations have been linked previously to the development of resistance to the drug venetoclax in some leukemia patients.
Using GoT-Splice, the researchers also found MDS-like changes in the marrow cells of people with a symptomless condition called clonal hematopoiesis (CH) – a mildly abnormal proliferation of one blood cell type – in this case involving SF3B1 mutations.
“That finding in CH patients suggests that the line between CH and overt disease can be more quantitative than qualitative – if the clone of abnormal cells is relatively small, then the rest of the bone marrow can compensate,” said Landau, who is also a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine.
He and his team plan to keep using GoT-Splice as a versatile tool for revealing the details of how gene mutations lead to disease.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see profile for Landau.
Jim Schnabel is a freelance writer for Weill Cornell Medicine.
Media Contact
Eliza Powell
Get Cornell news delivered right to your inbox.
Subscribe