Childhood HIV vaccination strategy shows promise in study
By Wynne Parry
Research at Weill Cornell Medicine suggests that childhood immunization against HIV could one day provide protection before risk of contracting this potentially fatal infection dramatically increases in adolescence.
The study, published Aug. 30 in Science Immunology, demonstrated that a series of six vaccinations containing a modified protein from the surface of HIV particles stimulated initial steps of a potent immune response in young nonhuman primates. This difficult-to-achieve response represents an important step toward providing full and potentially lifelong protection against the virus, the researchers say.
Immunizing young children, rather than adults, makes sense because risk factors for HIV infection rise steeply when adolescents become sexually active, according to senior author Dr. Sallie Permar, the Nancy C. Paduano Professor in Pediatrics and chair of the Department of Pediatrics at Weill Cornell Medicine.
Evidence also suggests that the immune systems of infants and children generally mount more effective responses to the virus than those of adults. Said Permar: “One of the advancements we’ve made is to demonstrate that an HIV vaccine could be delivered on a schedule similar to routine vaccines already given to babies and children.”
HIV predominantly infects immune cells called CD4 T cells, leaving individuals vulnerable to opportunistic diseases. Without lifelong treatment, infection is fatal. In 2022, an estimated 140,000 adolescentsbetween ages 10 and 19 worldwide became infected with the virus – a group that is overrepresented in the number of new infections.
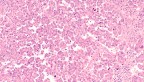
Vaccine researchers are seeking ways to stimulate the immune system to make “broadly neutralizing antibodies” against the virus before a person is exposed to it. These antibodies attack a crucial part of the HIV virus – the protein on its surface that binds to CD4 T cells. In doing so, broadly neutralizing antibodies prevent many strains of HIV from entering the cell and infecting it.
In this study, the researchers started with an experimental vaccine developed previously from spike proteins on the envelope of HIV particles. Study authors John Moore, a professor of microbiology and immunology, and Rogier Sanders, an adjunct associate professor of research in microbiology and immunology at Weill Cornell Medicine and a professor at Amsterdam UMC, sought to improve this vaccine by altering the viral protein. They designed these changes to stimulate a specific set of antibody-producing B cells that protect CD4 T cells.
“An effective HIV vaccine needs to engage the right set of B cells in order to generate a broadly protective response,” said first author Ashley Nelson, an assistant professor of immunology research in pediatrics. “We discovered that introducing certain mutations into the envelope protein could accomplish that in the setting of a naïve immune system.”
The researchers administered the modified vaccine to five young primates in three priming doses, starting less than a week after birth. They followed these with three doses of the vaccine matching the original HIV envelope protein, with the last dose given when the animals reached 78 weeks old, roughly equivalent to 4 or 5 years old for a human. As a control, five animals received all six doses of the original envelope protein vaccine.
“While exposure to the modified protein got the immune response started off in the right direction, booster shots containing the original version of the viral protein were necessary to reach full potential,” Nelson said.
Three of the five animals that received the modified version of the priming vaccine developed antibodies that appeared to be precursors to the sought-after broadly neutralizing response. Tests suggested these antibodies attacked the site the virus uses to invade CD4 T cells. However, they were not yet fully effective against the same breadth of HIV strains as mature, broadly neutralizing antibodies. One of the three animals also showed signs of developing the mature, broadly neutralizing response.
The next step, Nelson said, is figuring out how to reliably elicit a full-on broadly neutralizing response. “We still need to identify the right combination of viral proteins to get us further down that path,” she said, “starting from the earliest stages in life when multi-dose vaccines are commonly given.”
This work was supported by grants from the National Institutes of Health.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, please see the profile for Dr. Sallie Permar.
Wynne Parry is a freelance writer for Weill Cornell Medicine.
Media Contact
Barbara Prempeh
Get Cornell news delivered right to your inbox.
Subscribe