Lawrence Bonassar, the Daljit S. and Elaine Sarkaria Professor in Biomedical Engineering, brings new insight into the mechanism and efficacy of hyaluronic acid treatment for arthritis.
Study could inform debate over arthritis treatment regulation
By Syl Kacapyr
The debate over how one of the most popular osteoarthritis treatments should be federally regulated could change, thanks to a Cornell study providing a better understanding of the science behind hyaluronic acid (HA) injections.
The medical community has been divided over exactly how HA injections provide pain relief to osteoarthritis patients. HA products, typically injected into the knee, replace naturally occurring HA that has been depleted, lubricating the joints and preventing bones from rubbing together.
These injections, used for arthritis treatment for more than 30 years, constitute a $1 billion market in the U.S. The products are currently classified by the U.S. Food and Drug Administration (FDA) as class III medical devices, meaning pain relief is achieved through mechanical actions – mainly the reduction in friction between the bones – as opposed to chemical actions.
But in December 2018, the FDA declared its intention to consider reclassifying HA products as drugs, citing scientific evidence that suggests HA achieves pain relief through chemical actions within the body. If reclassified, new HA products would face a much steeper challenge in reaching the market, affecting treatment options for the 30 million people in the U.S. who have osteoarthritis.
A new study led by Lawrence Bonassar, the Daljit S. and Elaine Sarkaria Professor in Biomedical Engineering and in Mechanical and Aerospace Engineering, provides new insight on HA’s mode of action. The researchers found the mechanical properties provided by HA’s viscosity, specifically its ability to effectively lubricate cartilage, correlate much more directly to clinical efficacy – i.e., pain relief – than previously thought.
The research, “Frictional Characterization of Injectable Hyaluronic Acids Is More Predictive of Clinical Outcomes Than Traditional Rheological or Viscoelastic Characterization,” was published May 10 in the journal PLoS One. Edward Bonnevie, M.S. ’15, Ph.D. ’16 (mechanical engineering), currently a postdoctoral researcher at the University of Pennsylvania, was lead author.
“Researchers have typically used rheometry [the measurement of flow and deformation] to measure how HA reacts to applied forces and to predict its clinical performance, but our study shows it’s a poor predictor,” Bonassar said. “A lot of the disagreement over how HA works is rooted in the fact that, until now, there hasn’t been a better test of how mechanical properties predict performance.”
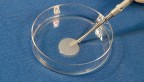
To test the viscosity of six different HA products, Bonassar’s team engineered a custom tribometer – a device used to measure coefficient of friction – that rubs cartilage back and forth on a glass plate and measures friction and how the products affect it.
“What we found was that each product’s lubricating properties directly correlated with the amount of pain relief reported in patient surveys. This is the first time anyone has been able to show such a clear correlation, and it suggests the debate over how HA works has been somewhat misinformed,” said Bonassar, suggesting that more research should be conducted before a decision is reached on HA treatment regulation.
Bonassar said the study also provides an effective framework from which new HA formulations can be tested, potentially leading to better products and treatment options for those with osteoarthritis.
The study was co-authored by scientists from Fidia Farmaceutici S.p.A. of Padua, Italy, and supported by the National Science Foundation Graduate Research Fellowship program.
Syl Kacapyr is public relations and content manager for the College of Engineering.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe