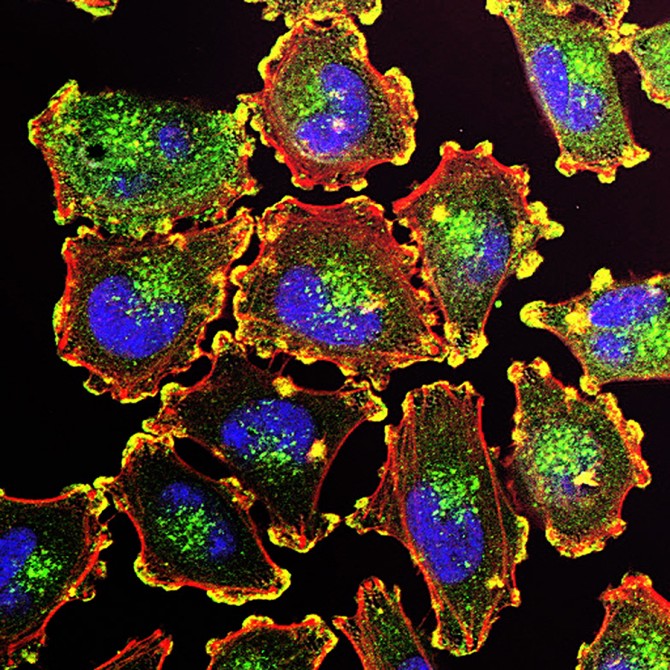
How melanoma cells escape oxidative stress to metastasize
By Bridget Kuehn
Investigators from Weill Cornell Medicine have discovered a defense mechanism that protects skin cancer cells from oxidative stress and helps them spread. The findings suggest a new drug target that could lead to therapies for deadly metastatic skin cancer.
When cancer cells colonize vital organs, they enter hostile territory, making it difficult to metastasize. Melanoma cells, for instance, experience high levels of oxidative stress in the bloodstream and at distant sites that kill most metastasizing cells before they can form new tumors. But what enables cancer cells to escape the effects of oxidative stress and spread?
A study, published Oct. 22 in Nature Cancer, details a mechanism that allows metastasizing melanoma cells to withstand this stress. While the proteins in the body are usually constructed from 20 common amino acids, the researchers identified an enzyme called FTSJ1 that chemically tags the tRNA molecule carrying the 21st amino acid, selenocysteine. This modification called methlyation prompts the cancer cells to produce selenocysteine-containing proteins to cope with oxidative stress.
“We dove into the unique biology of selenocysteine protein assembly and found a process that plays a central role in melanoma metastasis,” said senior author Elena Piskounova, assistant professor of cell biology in dermatology at Weill Cornell Medicine. “Melanoma cells lacking the FTSJ1 enzyme are more sensitive to damaging oxidative stress, so developing therapies that target FTSJI could help us prevent or treat metastasis.”
First author Leona Nease was a graduate student in the Piskounova lab when she conducted this research.
This new study builds on Piskounova’s previous research which demonstrated oxidative stress suppresses metastasis in melanoma. However, the current paper showed that some metastatic cells have increased levels of FTSJ1, which in turn increases the production of selenoproteins and the potential for these cells to metastasize.
“It’s become clear that metastatic cancer cells don’t rely on genetic mutations, but on reversible epigenetic, metabolic, or other processes that enable these cells to adapt to changing conditions,” said Piskounova, who is also a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine.
Working with laboratory grown melanoma cells and animal models, the researchers found that knocking out FTSJ1 turned off the defense mechanism, making melanoma cells vulnerable to oxidative stress. Indeed, FTSJ1 is necessary for promoting metastasis in animal models of melanoma.
The results suggest that therapies targeting FTSJ1 may prevent or treat metastasis with few side effects to normal tissues since FTSJ1 is only needed during early brain development. Blocking metastasis is critical since the five-year survival rate for people whose melanoma is detected and treated before it spreads is greater than 99% but drops to 35%, once the cancer has spread to other organs, according to the American Cancer Society.
Currently, Piskouvnova and her colleagues are working on developing small molecules that inhibit FTSJ1. They also want to repeat their studies in pancreatic cancer cells to determine if similar mechanisms control metastasis in other types of cancer. “Scientists often overlook selenocysteine protein biology, so it is exciting to discover it plays a key role in something as clinically important as metastasis,” she said.
This work was supported in part by American Cancer Society, Elsa U. Pardee Foundation Grant and Feldstein Medical Research Foundation Award.
Bridget Kuehn is a freelance writer for Weill Cornell Medicine.
Media Contact
Barbara Prempeh
Get Cornell news delivered right to your inbox.
Subscribe