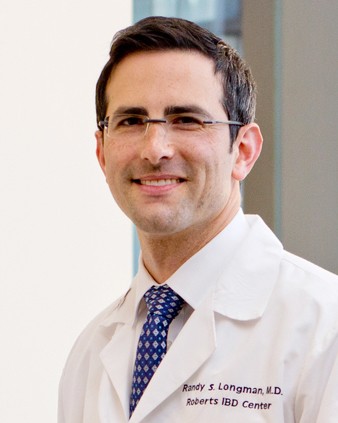
Dr. Randy Longman receives NIH Transformative Research Award
By Bridget Kuehn
Dr. Randy Longman, M.D. ’07, director of the Jill Roberts Center for Inflammatory Bowel Disease and an associate professor of medicine at Weill Cornell Medicine, and colleagues have received the NIH Director’s Transformative Research Award to develop the tools needed to understand how the gut microbiome drives metabolic pathways.
Established in 2009, the award funds innovative but inherently risky research endeavors that have the potential to overturn existing scientific paradigms or create new ones.
Part of the High-risk High-Reward program, it helps fund large-scale, unconventional projects that may create new research tools or technologies or develop radically different diagnostic or therapeutic approaches. The award will provide about $3.5 million over five years to Longman and his co-principal investigators Aaron Wright, the Schofield Endowed Chair in Biomedical Science and professor at Baylor University, and Chun-Jun Guo, assistant professor in the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine.
“The NIH Director’s Transformative Research Award identifies areas in science where there is an unmet need and an opportunity through collaborative science to make transformative breakthroughs,” Longman said. “It’s an exciting opportunity for three scientists with three distinct scientific programs to come together to accelerate our understanding of the functional impact of gut microbes on human health.”
Longman is a gastroenterologist and mucosal immunologist focused on understanding the causes of inflammatory bowel disease and developing new treatments. People with the disease have an altered gut microbiome, but the functional effects of these changes or how therapies like dietary changes might alter them are not yet apparent.
“Scientists have studied the microbiome for over a decade with advanced sequencing technologies, and we are very good identifying the microbes that make up the microbiome, genetically sequencing them, and recognizing the metabolites they produce,” Longman said. “Now, it’s really about connecting the dots between what the microbes are doing and how it affects human health.”
Wright, a chemist who has previously developed chemical probes to study the enzymes and proteins created by soil microbes, will make similar chemical probes that will allow the team to identify and track the source of proteins and enzymes produced by the gut microbiome. Guo will use his skill in genetically engineering gut microbes to tease apart what the proteins and enzymes do. They will use these techniques to understand the impact of therapies like increased fiber on the microbiome, which Longman is currently studying in clinical trials with patients with inflammatory bowel disease.
“Our goal is to understand which bacteria have major functional impacts and how we can leverage them to improve disease outcomes,” Longman said.
For example, Guo explained, once the chemical probes identify an enzyme of interest in human gut microbe samples, he can genetically engineer gut microbes that don’t produce the enzyme, or make too much of it, to see how that affects the gut in animal models. Guo said that the technology may lead to breakthroughs in treating inflammatory bowel disease and other conditions involving the microbiome.
“If this technology works, we can isolate microbes based on their function,” Guo said. “If we can then show that some of them are critical to modulating disease severity by reducing inflammation, these microbes could form the basis of a new microbiome-based therapy.”
Bridget Kuehn is a freelance writer for Weill Cornell Medicine.
Media Contact
Barbara Prempeh
Get Cornell news delivered right to your inbox.
Subscribe