Origin of deadly ovarian cancer identified
By Krishna Ramanujan, Cornell Chronicle
Researchers have identified the origin of ovarian cancer that develops in the fallopian tube, which opens doors to discovering new methods for diagnosing the disease and potential therapies.
The cancer, called high-grade serous carcinoma, is the chief and most aggressive form of ovarian cancer, the sixth-leading cause of death from cancer in women, with most patients dying within five years of detection. There are no symptoms, and no diagnostic tools have existed for early detection.
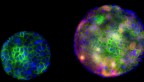
Scientists knew little about its origins, but a new study published Oct. 5 in Nature Communications identifies a transitional cell in the fallopian tube – called pre-ciliated tubal epithelial cells – as being especially cancer-prone.
Pre-ciliated cells develop from stem cells and are intermediaries in the lineage between stem cells and their final state, called ciliated cells, which allow movement of fluids and eggs in the fallopian tube.
“We not only identified cells where the cancer originates, but we identified mechanisms which can be potentially used for new therapeutics and new diagnostic tools,” said Dr. Alexander Nikitin, professor of pathology in the Department of Biomedical Sciences in the College of Veterinary Medicine and the paper’s senior author.
The study was done in mice. The fallopian tube in humans is called an oviduct in mice, so the researchers called it a uterine tube in order to refer to the same structure in both species. High-grade serous carcinoma develops in both the ovary and a part of the uterine tube. While previous work by Nikitin and colleagues has identified the origins of this cancer in the ovary, this is the first time they are identifying cancer-prone cells in the uterine tube.
The study’s first step characterized all the cell types found in the uterine tube, which had not been previously known. “The question was, to what extent all of the cells contribute to ovarian cancer,” Nikitin said.
Nikitin and colleagues also knew that in human high-grade serous carcinomas a gene called TP53 (Trp53 in mice) is mutated in more than 96% of cases, while different components of a pathway controlled by another gene called retinoblastoma 1 (RB1 in humans, Rb1 in mice) are altered in more than 60% of cases. Both genes suppress tumors when working properly.
In previous research on high-grade serous carcinoma in the ovary, stem cells were a main culprit for cancer development after inactivation of Trp53 and Rb1. In the section of the uterine tube that this study focused on, called the distal tubal epithelium, stem cells differentiate to become either secretory or ciliated cells.
The researchers found no cancer developed, even a year after the treatment, when Trp53 and Rb1 were silenced in stem cells of engineered mice, revealing that such cells themselves were not the source of the cancer. Instead, they found the stem cells died after inactivation of either Trp53 alone or together with Rb1.
“They simply cannot live without Trp53, so instead of transforming cells, you eliminate them,” Nikitin said.,
The researchers noticed that high-grade serous carcinomas were formed in an engineered mouse after inactivation of Trp53 and Rb1 in cells expressing a gene called Pax8. Using computational analysis based on single-cell sequencing data, they looked for cells that were not stem cells but that expressed Pax8.
“We found there is a population of cells that really fits these criteria,” Nikitin said. “And the cells turn out to be premature cells of ciliogenesis, or pre-ciliated transitional cells.”
The pre-ciliated cells are characterized by expression of several genes that are very specific for different stages of the cell’s own development. One such gene, Krt5, is specific to these pre-ciliated transitional cells. In another line of engineered mice, the researchers inactivated Trp53 and Rb1 in Krt5 pre-ciliated cells, and found the mice efficiently formed high-grade serous carcinomas.
Ciliogenesis, or the formation of cilia, is well-studied, Nikitin said, which will make it easier to find potential diagnostic and therapeutic targets.
Co-authors include John Schimenti, the James Law Professor of Genetics in the Department of Biomedical Sciences in CVM; and Benjamin Cosgrove, associate professor in the Meinig School of Biomedical Engineering in Cornell Engineering. Andrea Flesken-Nikitin, an assistant research professor in Nikitin’s lab, and Coulter Ralston, a doctoral student in Nikitin’s and Cosgrove’s labs, were co-first authors of the paper. Researchers from the University Children’s Hospital in Zurich, Switzerland; and the Memorial Sloan Kettering Cancer Center in New York City were also collaborators.
The study was funded by the National Institutes of Health, the Ovarian Cancer Research Fund, the Sandra Atlas Bass Endowment for Cancer Research and the National Science Foundation.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe