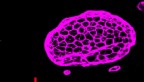
Researchers used two-photon microscopy to image pyramidal tract neurons and discovered this cell type is essential for psilocybin’s long-term behavioral effects.
Hitting the target: Imaging reveals psilocybin’s neural odyssey
By David Nutt, Cornell Chronicle
Psilocybin is the active ingredient that gives so-called “magic mushrooms” their hallucinogenic kick. It also has a therapeutic potential for treating depression.
Cornell researchers have identified a pair of key neurological mechanisms in the brain – a cell type and receptor – that enable the psychedelic compound’s long-lasting effects.
Targeting the pyramidal tract neurons and their specific serotonin 5-HT2A receptor in the medial frontal cortex could enable pharmaceuticals to deliver psilocybin’s mood-altering benefits while suppressing the perceptual hallucinatory trip.
The findings were published April 2 in Nature. The study’s co-lead authors are postdoctoral researcher Ling-Xiao Shao and Clara Liao, a doctoral student at the Yale University School of Medicine, both of whom work in the lab of senior author Alex Kwan, Ph.D. ’09, associate professor of biomedical engineering, who led the project.
Kwan’s lab uses high-resolution optical imaging to better understand how psychedelics remodel the brain’s circuitry. In 2021, his team showed that psilocybin induces structural plasticity – the brain’s ability to reshape its structure – particularly with the rapid growth of dendritic spines, which form the basis of synaptic connections.
“Building off that previous study, we wanted to see where the neuronal connections are grown in the different cell types in the brain,” said Kwan, who has a secondary appointment as associate professor of biomedical engineering in psychiatry at Weill Cornell Medicine. “We started playing around with these cell types, and we asked: Which are important for psilocybin’s behavioral effects? If we silence some of these neurons, will psilocybin still be able to do its thing and be therapeutic?”
Using two-photon microscopy on transgenic mice, the researchers targeted the two largest populations of primary cells in the brain: pyramidal tract (PT) neurons and intratelencephalic (IT) neurons.
Inactivating the IT neurons, which are responsible for high-order cortical-cortical communication, did not change the behavioral effects of the psilocybin. But when the researchers silenced the PT neurons, the drug was essentially ineffective – proof that this cell type and its pathway, which extends from the frontal cortex down into the midbrain and brainstem – is essential to psilocybin’s effects.
Equally important is the PT neurons’ 5-HT2A receptor, which has previously been shown to play an important role in humans experiencing acute, short-term hallucinatory trips. When the researchers knocked out the receptors, psilocybin’s positive behavioral effects disappeared. None of their manipulations affected the acute effects.
“This suggests that it’s really the same serotonin 2A receptor that is also quite important for the long-term behavioral effects,” Kwan said. “The brain circuitry is where it differs.”
Essentially, the frontal cortex is important for therapeutic effects, whereas the subjective perceptual effects – i.e., “the trip” – likely rely on another region of the brain, such as visual pathways. This could have important implications for pharmaceutical treatment.
“Right now, a huge focus from the pharmaceutical companies is on developing drugs that may be able to take out the trip but still give you the benefit for treating mental illnesses,” Kwan said. “But what this work shows is that that could be difficult, because in the end, they target the same receptor. So one might think about just delivering the drug to some specific brain areas, which can be a better way to do it.”
Other contributors included postdoctoral researchers Ling-Xiao Shao, Quan Jiang, Samuel Woodburn and Olesia Bilash; Cassandra Wojtasiewicz ’23, Diran Tan ’25 and Jack D. Nothnagel ’25; Hail Kim of Korea Advanced Institute of Science and Technology; and Alicia Che, Rong-Jian Liu, Pasha Davoudian and Neil Savalia of Yale University School of Medicine.
The research was supported by the National Institutes of Health; a One Mind–COMPASS Rising Star Award; Source Research Foundation; and the Connecticut Department of Mental Health and Addiction Services.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe