Clinical test validates precision medicine for cancer
By Renee Twombly
Much of precision medicine and cancer care focuses on targeting the genomes of specific tumors or metastases. A Weill Cornell Medical College research team has now shown that a more global look at the body using next-generation sequencing can offer new insights and treatment targets in patients with advanced, treatment-resistant disease.
The research, published May 28 in JAMA Oncology, offers a look at how the Institute for Precision Medicine at Weill Cornell and NewYork-Presbyterian Hospital is transforming the way physician-scientists address individualized cancer care.
“Most institutions are using focused or panel sequencing to look at a few hot spot mutation areas in cancer,” said senior author Dr. Mark Rubin, the institute's director, and the Homer T. Hirst III Professor of Oncology in Pathology and a professor of pathology and laboratory medicine at Weill Cornell. “But we believe that Whole Exome Sequencing, which tests more than 21,000 genes in the cancer's exome, the DNA that is transcribed into RNA, is ideal for patients with advanced cancer where we don't know where the mutations of resistance are.”
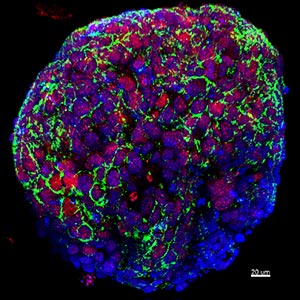
To conduct their research, Rubin, lead author Dr. Himisha Beltran and their team of investigators developed a clinical trial and enlisted 97 cancer patients with advanced, treatment-resistant disease. All participants consented to testing their metastatic disease genome as well as their normal tissue with a Whole Exome Sequencing clinical test called EXaCT-1, which was developed at Weill Cornell. The team also developed three-dimensional cancer cells known as organoids from each individual biopsy, as well as xenografts - cancer tissue samples - for animal study, which allowed them to review the genetics of the disease and to test treatments.
“These are patients who had exhausted every treatment option available to them,” said Beltran, an assistant professor of medicine at Weill Cornell. “But with Whole Exome Sequencing - and reviewing the cancer's exome, which is believed to harbor the vast majority of mutations that drive disease - we were able to identify new therapeutic possibilities.”
The team examined 154 tumors from the 97 patients and found an average of 16 mutations per patient. Of the mutations, 16 could be immediately targeted by available drugs, 98 had targeted therapies in clinical or preclinical development and 1,474 will require additional research to understand their clinical or biological significance.
Patients and their clinicians were informed of the results through an EXaCT-1-generated report. A multidisciplinary precision medicine tumor board, which reviewed the patients' genomic sequencing results, medical histories and radiology reports, developed and shared treatment recommendations for 92 percent of the cases.
The board's recommendations led to a positive outcome for one patient with advanced bladder cancer after a combination therapy successfully reversed the disease's spread to the lungs and liver. Another patient with an aggressive form of prostate cancer went into complete remission during the study, and the investigators used genomic data to understand why he experienced this exceptional response to the common chemotherapy he'd received.
“The dramatic and durable remission that a neuroendocrine prostate cancer patient experienced, even after several years of follow-up, is exceptional,” Rubin said. “This study shows what is possible, both in terms of treatment and advanced learnings, with precision medicine.”
But while their study highlighted the promise of precision medicine, it also revealed some challenges: Only 5 percent of cases could follow the tumor board's recommendations, Beltran said.
“This was largely because patients did not have access to the recommended therapies through clinical trials or because the drug was not available,” she said, a challenge rooted in the field's infancy.
“Yet our study also demonstrates the feasibility of doing an extensive molecular analysis within a short time frame in order to find potential therapies that had not been used before,” she added. “This is an accomplishment that brings us closer to realizing our goal.”
Renee Twombly is a contributing writer for Weill Cornell Medical College Office of External Affairs.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe