Researchers test using AI to optimize IVF embryo selection
By Jamie Kass
A new artificial intelligence approach by Weill Cornell Medicine investigators can identify with a great degree of accuracy whether a 5-day-old, in vitro fertilized human embryo has a high potential to progress to a successful pregnancy.
The technique, which analyzes time-lapse images of the early-stage embryos, could improve the success rate of in vitro fertilization (IVF) and minimize the risk of multiple pregnancies.
The group’s paper, “Deep Learning Enables Robust Assessment and Selection of Human Blastocysts After In Vitro Fertilization,” published April 4 in NPJ Digital Medicine, a publication of Nature.
Infertility is estimated to affect about 8 percent of women of childbearing age. While IVF has helped millions give birth, the average success rate in the U.S. is approximately 45 percent.
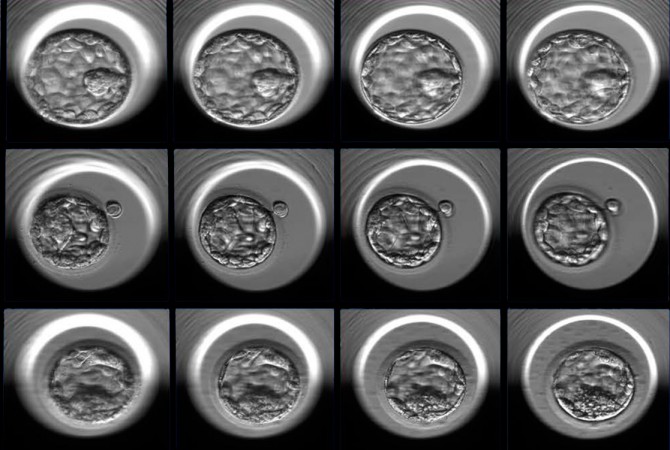
For the study, investigators used 12,000 photos of human embryos taken precisely 110 hours after fertilization to train an artificial intelligence algorithm to discriminate between poor and good embryo quality. To arrive at this designation, each embryo was first assigned a grade by embryologists, based on various aspects of the embryo’s appearance.
The investigators then performed a statistical analysis to correlate the embryo grade with the probability of going on to a successful pregnancy outcome. Embryos were considered good quality if the chances were greater than 58 percent and poor quality if the chances were below 35 percent.
After training and validation, the algorithm, dubbed Stork, was able to classify the quality of a new set of images with 97 percent accuracy.
“By introducing new technology into the field of IVF we can automate and standardize a process that was very dependent on subjective human judgement. This pioneering work gives us a window into how this field might look in the future,” said Dr. Zev Rosenwaks, director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at NewYork-Presbyterian/Weill Cornell Medical Center and Weill Cornell Medicine, and the Revlon Distinguished Professor of Reproductive Medicine in Obstetrics and Gynecology at Weill Cornell Medicine.
Choosing the embryo with the best chance of developing into a healthy pregnancy is currently a subjective process. Even experienced embryologists rarely agree on how to predict the viability of an individual embryo based upon its appearance at the blastocyst stage – 110 hours, approximately five days, after fertilization – at which it consists of only 200 to 300 cells.
“We wanted to develop an objective method that can be used to standardize and optimize the selection process to increase the success rates of IVF,” said Nikica Zaninovic, co-senior author and director of the Embryology Lab in the Center for Reproductive Medicine.
In a collaboration between the Center for Reproductive Medicine and the Caryl and Israel Englander Institute for Precision Medicine at Weill Cornell Medicine, the investigators spent more than six months reviewing approximately 50,000 anonymized images, representing 10,148 human embryos, collected by time-lapse photography over seven years. With the embryologist-assigned grade and the hindsight knowledge of the pregnancy outcome, the investigators could classify the embryos as good, fair or poor quality. Ultimately, they used two sets of 6,000 images, good or poor quality, to teach the algorithm how to classify new images presented to it.
“This is the first time, to our knowledge, that anyone has applied a deep learning algorithm on human embryos with such a large number of images,” said Pegah Khosravi, the lead author of the study and a postdoctoral associate in computational biomedicine.
Deep learning is an artificial intelligence approach that is roughly modeled after the neural networks of the brain, which analyze information in increasing layers of complexity. The size of the training data set is critically important to the success of the algorithm, with more data leading to better outcomes.
“Our algorithm will help embryologists maximize the chances that their patients will have a single healthy pregnancy,” said Olivier Elemento, director of the Englander Institute for Precision Medicine and associate director of the HRH Prince Alwaleed Bin Talal Bin Abdulaziz Alsaud Institute for Computational Biomedicine at Weill Cornell Medicine. “The IVF procedure will remain the same, but we’ll be able to improve outcomes by harnessing the power of artificial intelligence.”
Stork is currently an investigative tool and the researchers plan to incorporate additional clinical and technical parameters to improve the algorithm.
“It’s very important that we could put a team together here that contains computer scientists, precision medicine experts, embryologists and clinicians,” said Dr. Iman Hajirasouliha, co-senior author and assistant professor of computational genomics in computational biomedicine in the HRH Prince Alwaleed Bin Talal Bin Abdulaziz Alsaud Institute for Computational Biomedicine, assistant professor of physiology and biophysics and a member of the Englander Institute for Precision Medicine. “We needed a strong team with a wide area of expertise to solve this problem.”
Jamie Kass is a science writer at Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe